Substance-Related and Addictive Needs
Adolescence is characterized by neurocognitive development, expanding social networks and attraction to novel situations. These factors can increase risky behavior, including substance misuse. Negative outcomes can be minimized with support and guidance from parents, caregivers and trusted professionals. Substance use disorder (SUD) is a pediatric disease that can affect individuals of all socioeconomic statuses.
Role of the Primary Care Provider:
Primary care practitioners (PCPs) and adolescent medicine health professionals are uniquely situated to manage SUDs; there is growing evidence that prevention and treatment should focus on substance use as a medical health condition, and the longitudinal, preventive and family/patient-centered care interventions that are the cornerstone of pediatric care should be applied. Growing evidence also supports the need for integration of SUD treatment into primary care.
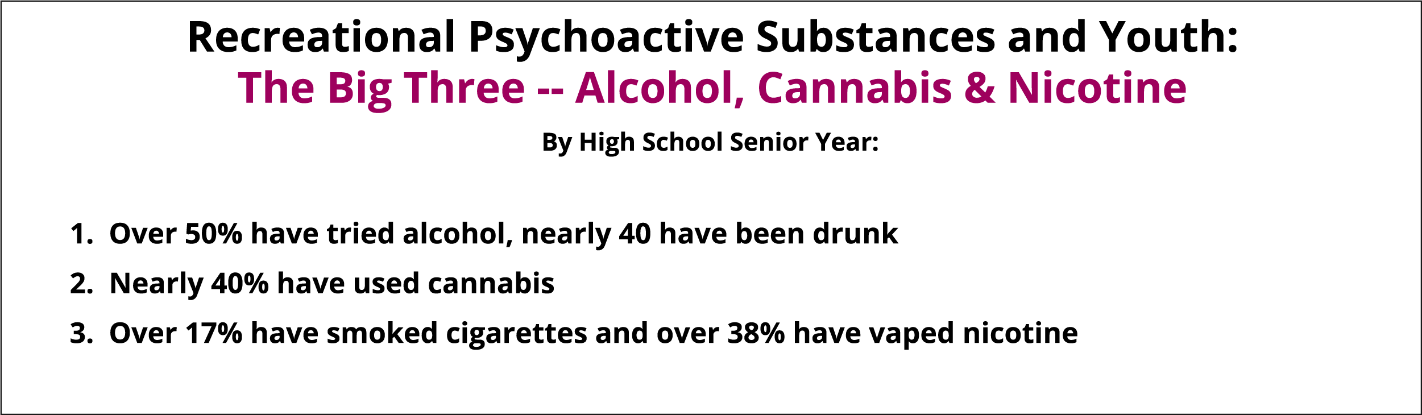
Alcohol, tobacco and marijuana are the substances most frequently used by adolescents. However, misuse of prescription opioids remains a significant issue in many communities. Amphetamines and other prescription drug use are also prevalent in this population (Volkow, 2014).
Risk of Adolescent Substance Abuse Use
- Academic underachievement
- Legal system involvement
- Teen pregnancy
- STDs
- Violence
- Perpetration
- Victimization
- Injuries
- Exacerbated mental health difficulties
- Family conflict
- Peer difficulties
- Substance use problems lasting into adulthood
- Overdose
The younger a child is when substance use is initiated, the greater the likelihood of immediate and lifelong problems. Delaying the age at which children start experimenting with substances or intervening early to stop substance use when it starts, are important strategies to prevent SUD and minimize the associated short and long-term negative effects. In addition to significant acute risks, those who progress to using drugs intravenously face the additional risks of contracting comorbid hepatitis C and HIV. Early intervention is particularly crucial for opioid and tobacco use, where progression from limited use to addiction is faster than with other substances.
MYTH: Marijuana is not addictive and regular use will not have long-term effects on functioning.
Fact: Research has shown that regular marijuana use in adolescence increases subsequent subclinical psychotic symptoms significantly. Particularly, symptoms of paranoia and hallucinations may endure after continued abstinence.
The adolescent brain is undergoing significant development from ages 12-25. Research has also shown that long term or heavy marijuana use in adolescence is associated with altered brain development and cognitive impairment.
Clinical Pearl – Reducing Stigma
The stigma associated with substance use is one of the greatest barriers to treatment and recovery. Individuals with SUD often feel guilty and less deserving of help than individuals with other health conditions, as it has often been viewed as a “moral failing” instead of the chronic neurologic disease that it is. Providers who communicate a non-judgmental approach to treating substance use as a medical condition can dramatically improve the chances of obtaining accurate details of substance use and engaging patients and caregivers to make changes and improve outcomes.
1/4
Meet Sebastian
Sebastian is a 16-year-old boy who is brought to his primary care provider’s office to establish care. He was placed with a new foster family about 4 months ago and has a history of multiple foster placements since the age of 8. There are allegations of abuse and neglect from his biological family, with whom he no longer has contact. His foster parents are concerned about his mood, school truancy and defiant behavior. In addition to a PHQ-9 to screen for depression, the primary care provider uses a HEADSSS assessment and CRAFFT questions to survey his social history. In doing so, cannabis and opioid use is revealed.

1/3
Meet Mark
Mark is a 15-year-old male with no past medical history who presents for his well child check. Mark’s dad reports that he has been healthy and involved in football this year. His only concern is Mark’s grades. His grades have dropped from an A or B average to a C or D average. Mark is unconcerned about his grades and says that he will try harder next semester.

Prevention
Tobacco Use and Prevention
The leading cause of preventable death in the United States is tobacco product use and most tobacco use begins before the age of 18. While tobacco use has declined among school-aged children, use of e-cigarettes or vaping devices has increased. In 2020, 19.6% of high school students and 4.7% of middle school students reported using e-cigarettes. Nicotine exposure during adolescence can have long term effects on brain function, cognition, attention span, and mood. Education and brief counseling on tobacco use prevention by clinicians has been shown to be moderately effective at preventing initiation of tobacco use in school-aged children and adolescents. Primary care providers can offer resources to assist with both mental and physical aspects of nicotine addiction, including nicotine replacement therapy when appropriate.
Ohio Tobacco Quit Line: 1-800-QUIT-NOW (1-800-784-8669): Provides personal quit coaching and telephone counseling free of charge to ALL Ohioans. Nicotine patches, gum, or lozenges are provided for up to eight weeks at no charge to eligible participants.
Smokefree Teen: Offers tools & tips, access to live online help from National Cancer Institute information specialists, and free download of the quitSTART app.
Truth Campaign: Information and resources designed specifically for adolescents. Includes testimonials and 24-hour text-to-quit service to support teens in their quit attempt.
Effective prevention strategies meet youth where they are:
- For youth that report abstinence
- Provide patient and family education and positive reinforcement to maintain abstinence.
- For youth that report experimental or limited use
- Given clear medical advice and educational counseling to promote cessation
- Consider motivational interviewing strategies that emphasize strengths, personal goals, and self-efficacy as a basis for behavior change.
- Be aware of common risk factors (link below) for substance use disorder and make appropriate suggestions or referrals that promote protective factors and address patient risk.
- Given clear medical advice and educational counseling to promote cessation
Common Risk and Protective Factors for Substance Use Disorder
| Risk Factors | Protective Factors |
|---|---|
|
Trauma Family History Peer Influence Academic Failure Mental Health |
Monitoring Social Connectedness Management of psychiatric disorders |
Screening and Assessment
Screening
The American Academy of Pediatrics (AAP) and the Substance Abuse and Mental Health Services Administration (SAMHSA) recommend universal screening for drug and alcohol use with adolescents ages 12 and over in primary care settings. A substance use screen can be integrated into existing health and wellness screenings using a validated screening tool at both well visits and acute-care examinations.
Clinical Pearl: Dependence often Unrecognized
Adolescent opioid users experience progression from first use to dependence more quickly than adults, and may mistakenly attribute withdrawal symptoms to stress or illness. Providers should regard physical symptoms accompanying law enforcement, school, or mental health crisis events as potentially related to SUD. Those who report occurrences where substance use has created safety issues or interference with daily functioning should be referred for comprehensive assessment and treatment.
Screening, Brief Intervention and Referral to Treatment (SBIRT)
The Screening, Brief Intervention and Referral to Treatment (SBIRT) is an evidence-based approach developed for use in primary care settings to identify when patients are at risk of substance-related consequences that require early intervention and treatment services. SBIRT may be utilized as part of universal screening for all patients and can help to identify the severity of substance use and reinforce abstinence for appropriate patients.
SBIRT Steps
- SCREENING to identify level of substance use with standardized assessment tools and determine the appropriate treatment. It should be noted that standardized rating scales are neither definitively diagnostic, nor a definitive condition of specific condition. The intent is to determine if the symptoms experienced by the child are contributing to their social, emotional, behavioral, academic, or work challenges.
- BRIEF INTERVENTION (BI) to raise patient awareness of risks, provide feedback, and increase motivation for behavioral change.
- REFERRAL TO TREATMENT (RT) for patients whose screening identifies a need for specialized therapy or treatment.
The CRAFFT is a validated screening tool for adolescents aged 12-21 to help providers identify patterns of use and related issues:
- C: Have you even ridden in a CAR driven by someone (including yourself) who was “high” or had been using alcohol or drugs?
- R: Do you ever use alcohol or drugs to RELAX, feel better about yourself, or fit in?
- A: Do you ever use alcohol or drugs while you are by yourself or ALONE?
- F: Do you ever FORGET things you did while using alcohol or drugs?
- F: Do your family or FRIENDS ever tell you that you should cut down on your drinking or drug use?
- T: Have you ever gotten into TROUBLE while you were using alcohol or drugs?
Screening to Brief Intervention (S2BI)
A screening tool that can be used with the CRAFFT to assess the frequency of use and categorize substance use by adolescent patients into different risk categories. The accompanying resources assist clinicians in providing patient feedback and resources for follow-up.
Obtain a Substance Use History
Gather details of use for each substance whose use is reported. One brief way to do this in adolescents is to inquire about first use, last use, peak use, and current use. That is, 1) what age were they the first time they used the substance? 2) when did they most recently use the substance? 3) when have they used most frequently or intensely, how much or how often were they using? and 4) ask them to describe their current pattern (frequency, amount, and effects) of use.
Clinical Pearl: Diagnosis and Severity
While normative use of substances may vary among different populations, two key concepts in diagnosing and determining severity of SUDs in those who use substances are 1) continued use despite negative consequences, and 2) difficulty reducing or discontinuing use of the substance in those who wish to. Additionally, because motivation to change substance use can vary significantly, it is valuable to solicit information about the negative consequences of substance use from both the patient and the patient’s caregiver or other sources of collateral information. Some patients minimize both the frequency and intensity of their use and the negative consequences of their use; others may not fully connect substance use to its consequences (e.g., medical problems related to substance use over time, fights, or non-consensual sexual encounters while intoxicated).
Clinical Pearl: Relapse
Substance use disorder is a chronic, neurologic disease. Like other chronic diseases, periods of remission and relapse occur, and patients should continue to receive care at all points of their disease process.
2/4
Sebastian
Sebastian reports cannabis use is about once per month, but opioid use is almost daily. Sebastian endorses using oxycontin to relax, using oxycontin when alone, and getting into trouble due to using and stealing oxycontin. He also states that he uses escalating amounts of oxycontin to obtain the same high, experiences cravings, and spends increasing amounts of his time and energy to obtain or use oxycontin.
2/3
Mark
During his individual interview, Mark admits to using alcohol 2-3 times per month. Specifically, he reports drinking “a few beers and shots” on weekends during parties with his friends. The PCP asks for further details and Mark says that he will drink Friday nights until he “gets drunk” and then wake up late on Saturdays. He often feels too sick to get out of bed and cannot do his chores in the morning. He reports needing to “shake it off with some vodka” he keeps in his room. He will then go out on Saturday night and drink until he passes out. He tends to sleep late on Sundays as well and cannot focus on getting his homework done. He says he rarely drinks on weekdays. However, his friends on the varsity football team do drink after weekday practices and patient admits to sometimes letting those friends drive him home. He denies nicotine, marijuana, and other illicit drug use. His parents do not know about his drinking.
Diagnostic Criteria
The Diagnostic and Statistical Manual (DSM-5) characterizes SUD in terms of severity, based on the number of symptoms, and type of substance used (alcohol; cannabis; phencyclidine; hallucinogens; inhalants; opioids; sedatives, hypnotics; stimulants; tobacco; and other or unknown substances), with each labeled as a separate use disorder.
Meeting two or more criteria from the list below is categorized as SUD:
- Social or interpersonal problems related to use
- Failing to meet responsibilities at home, school, or work
- Experiencing withdrawal symptoms from use
- Use presents safety issues or danger to self (e.g., overdose, DWI)
- Tolerance developed to a substance
- Use increasing over time
- Failed attempts to control or quit use
- A significant amount of time is dedicated to use
- Physical or psychological health issues related to use
- Decreased participation in activities
- Experiencing cravings for substance
3/4
Sebastian
After gathering a history of opioid use, Sebastian’s primary care provider believes that he has an opioid use disorder. Sebastian displays several of the criteria for SUD: social problems related to use, failing to meet responsibilities/decreased participation in activities, withdrawal symptoms/cravings and tolerance/increasing use over time, and a significant amount of time dedicated to use. The primary care provider recognizes that this is a high-acuity situation and the need for intervention is imminent. The primary care provider praises Sebastian for divulging this information and assesses his readiness to make a change.
Treatment
Families should be urged not to rely on the common belief that youth can quit on their own without support. Providers can assist families in determining the right program for treatment that provides appropriate care in the least restrictive setting and is individualized with respect to experience, family and social support, and preferences. Patients who consent to treatment are more likely to participate and have better outcomes. When screening results suggest that an SUD may be present, providers should refer patients to a licensed chemical dependency counselor, if possible. A licensed chemical dependency counselor can complete a full diagnostic assessment and make treatment recommendations.
The following is an overview of evidence-based treatment approaches. Each approach targets specific aspects of adolescent SUD and includes a range of approaches that are aimed to impact individuals, families, and communities.
Behavioral Approaches
The goal of behavioral treatment is to change attitudes and behaviors about substance use, improve family communication and interactions, and increase healthy life skills and coping mechanisms.
Motivational Interviewing (MI)
MI is an evidence-based practice for patient-centered care that supports behavior change by empowering adolescents to make more positive and healthy choices. It has been shown to be an effective modality in the treatment of adolescent substance use.
MI relies on the use of open-ended questions and reflective responses to help patients examine their own behavior and identify ways to overcome perceived barriers. Behavior change often occurs as decisions made during stages of change, identified as precontemplation, contemplation, preparation, action, maintenance, and termination. Nonadherence with medical advice or treatment may be due to conflicts between treatment goals and the readiness or motivation of the patient to make changes
Motivational Interviewing and Stages of Change Resources
- Transtheoretical Model and Stages of Change Video
- Stages of Change Model in Addiction Recovery
- Substance Abuse and Mental Health Services Administration (SAMHSA) Guide for Motivational Interviewing
- SAMHSA Quick Guide for Enhancing Motivational Interviewing
Family-Based Approaches
Adolescent SUD treatment often includes family-based approaches, which may incorporate the parent(s), sibling(s), and peers. Some of the main concerns addressed in family-based approaches such as Intensive Home-Based Treatment, Functional Family Therapy, and Multidimensional Family Therapy include family communication and interaction, comorbid disorders, academic and vocational challenges, and social relationships.
Medication Assisted Treatment
Several medications are effective for the treatment of opioid, alcohol, and nicotine substance use disorders. While these evidence-based treatments do not all have FDA approval for use by adolescents, preliminary evidence suggests they are effective, and the risks associated with their use are no greater among adolescents than among adults. Healthcare professionals should be prepared to prescribe and/or refer patients for medications for treatment and relapse prevention in conjunction with behavioral health interventions.
Nicotine Use Disorders
Bupropion (Zyban) - FDA approved for adults. Acts by reducing nicotine cravings and withdrawal symptoms.
Nicotine Replacement Therapies (NRTs) - NRT’s work by activating nicotine receptors in the brain, thus aiding the process of weaning smokers off cigarettes. Available in the form of a patch, gum, lozenge, nasal spray, or inhaler. AAP recommends their off-label use for NRT for youth. They are most often prescribed as pairing a long-acting form (patch) with short acting form (gum, lozenge, spray, inhaler) to achieve optimal results.
Varenicline - FDA approved for adults. Mildly activates nicotine receptors in the brain, and therefore reduces nicotine cravings and withdrawal.
Alcohol Use Disorders
Acamprosate - Reduces withdrawal symptoms and prevents relapse by acting on brain pathways that are negatively impacted by chronic alcohol use.
Naltrexone - Available as an oral tablet or long-acting injectable, naltrexone works by decreasing the sense of euphoria experienced by alcohol users.
Opioid Use Disorders
The American Academy of Pediatrics Committee on Substance Use and Prevention (2016) recommends that PCPs consider offering medication-assisted treatment to their adolescent and young adult patients with severe opioid use disorders or discuss referrals to other providers for this service.
Buprenorphine - A partial opioid agonist that activates and blocks opioid receptors in the brain. Buprenorphine reduces withdrawal symptoms and cravings without producing the dangerous side effects of uncontrolled opioid use. Buprenorphine is approved for youth ages 16 and older and is available for single administration sublingually and in combination with naloxone. It may be prescribed by a pediatric primary care provider to support detoxification and ongoing maintenance therapy.
Methadone - A full opioid agonist that prevents withdrawal and reduces cravings. With a long-documented history in opioid treatment for adults, methadone is available for administration by licensed methadone treatment programs. In select cases and states, adolescents between the ages of 16 and 18 with an opioid use disorder may be eligible for methadone treatment.
Naltrexone - Naltrexone is approved for relapse prevention in adults who have completed detoxification. Naltrexone acts as an opioid antagonist by blocking opioid receptors. The medication prevents the typical high that a user would experience from drug use, as well as preventing withdrawal symptoms if opioid use has recently been stopped.
There are currently no FDA approved medications for the treatment of cannabis, cocaine, or methamphetamine use disorders in any age group.
Recovery Support Services
Recovery support services such as continuing care, mutual help groups, peer recovery support, and recovery high schools bring together individuals to share their experiences, provide reciprocal support to one another, and promote an abstinent lifestyle. While such services are not a replacement for the formal treatment services, they may be used in tandem with them.
Peer Recovery Support Services
Peer recovery support services pair individuals with groups and peer leaders who have experience with SUD. Depending on the needs of the adolescent, peer recovery support services may also be useful for connecting an individual with the necessary treatment resources,12-step groups, mentorship, or coaching. To aid in the building of healthy, non-substance related relationships, peer recovery support services may lead community activities for recovering adolescents as well.
4/4
Sebastian
After using some basic motivational interviewing techniques, Sebastian’s primary care provider determines that Sebastian is relieved at the prospect of getting help and is in the “action” stage of change. A referral is made for substance use treatment and Sebastian begins an intensive outpatient program (IOP) that provides MAT with suboxone. The program meets 2.5 hours/day three times a week for 2 months. After completing the IOP, Sebastian shifts to weekly outpatient substance use treatment and at his next appointment with his primary care provider he reports that he has been sober for four months. The primary care provider congratulates Sebastian on this success and his foster family for the support that they have provided. The primary care provider also discusses the steps they are all taking to help maintain Sebastian’s sobriety and reviews plans to handle a relapse if it occurs.
3/3
Mark
The PCP provides education regarding the health hazards of drinking. The PCP also asks Mark if he would be open to talking about his drinking, at which point he asks for help from the PCP. Together they are able to have an open conversation with Mark’s dad during the visit. Mark and his dad are provided with “A Contract for Life” to help Mark and his dad prevent unsafe driving situations. Lastly, the PCP scheduled a follow up appointment in one month to check on Mark’s progress and abstinence.
Confidentiality
The AAP statement Confidentiality in Adolescent Health Care gives guidance on the ethical obligation to include adolescents in conversations and decisions about their own health care apart from parents or guardians. Primary care physicians should be aware of state and federal confidentiality protections or adolescent patients and raise patient and family awareness of what types of services adolescents are able to access confidentially, such as mental health or substance use treatment, and situations where parent support may be helpful to patient well-being. Ohio revised code Section 3719.012 allows minors to give consent to diagnosis or treatment of a condition caused by a drug of abuse or alcohol. If the patient requests confidential services or treatments, providers should consider adjusting (if legal) where electronic health records, billing, or pharmacy reminders may inadvertently disclose PHI to parents or guardians. Accommodations may also need to be discussed if the patient is not intellectually or cognitively able to understand health information or provide informed consent on their own.
Clinical Pearl: Confidentiality and substance use
Disclosing substance use to parents of adolescent patients requires careful consideration. On one hand, care providers want to maintain an open and honest rapport to encourage disclosure. On the other hand, providers have a duty to ensure patient safety. There are also legal considerations. Under Ohio Law, patients 12 years and older are allowed to consent to their own substance use treatment. So, when is it okay to disclose substance use without the consent of the patient? When there are concerns about substantial risk and unsafe behaviors involving substance use it may be appropriate to discuss these concerns with parents. However, if there is concern that a patient may face extreme punishment or abuse if their parents are informed of their substance use, then it is advisable that the care provider avoids disclosure.
Where to Get Help
Ohio Mental Health and Addition Services Information and Referral Line
- If you need help, call 1-877-275-6364 for information and referral or text 4Hope to 741 741 to start a conversation with a person who is trained to help.
Call the Ohio CareLine: 1-800-720-9616
- The Ohio CareLine is a toll-free emotional support call service created by the Ohio Department of Mental Health and Addiction Services. Open 24 hours a day, 7 days/week for confidential support and connection to local providers.
Contact Your ADAMH Board (Ohio Association of County Behavioral Health Authorities (oacbha.org))
- Use the Ohio Association of County Behavioral Health Authorities (OACBHA) website to find your local board and get information about mental health and recovery support services in your community.
Substance Use Treatment Finder (Treatment Finder)
- The Treatment Finder website, sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA), can be used to identify treatment in your community. You can refine your search to identify age-specific services for youth.
Overdose Prevention: What to do in an emergency: CALL 911
- See this detailed set of instructions in case of an overdose emergency.
Opioid Overdose may occur with any use and requires immediate intervention to address respiratory depression and prevent respiratory arrest and death.
- Call 911
- Administer Naloxone: Narcan is an FDA approved nasal spray that can be used by professionals or nonprofessionals in the case of an opioid overdose. For instructions on how to properly deliver Narcan, visit this link on administering Narcan
Ongoing Support
PCPs and other health professionals play an important role in the treatment of SUD by providing or arranging treatment and monitoring progress through more frequent follow up appointments.
Family Support
Family members can contribute to a child or adolescent’s ongoing recovery by limiting triggers in the environment, setting appropriate boundaries, attending family therapy if it is suggested by the treatment team, making sure the child or adolescent attends treatment-related appointments, and promoting a healthy and balanced lifestyle. The following resources are recommended:
- AACAP.org: Substance Abuse Treatment for Children and Adolescents: Questions to Ask
- Adolescenthealth.org: Substance use resources for parents
Make a Safety Plan
- Overdose remains a major cause of mortality among youth; overdose education should be provided as part of any visit in which a youth reports opioid use.
- Naloxone can be obtained by family members of patients who may be likely to use opioids in case an overdose does occur. Visit this link for more information on naloxone regulations and how to obtain this life-saving medication.
Relapse Prevention
- SUD is a condition with a high risk for relapse. Clinicians, families, and others involved in the support system can help formulate relapse prevention plans.
Frequently Asked Questions (FAQs)
How can parents or caregivers help promote substance use prevention at home?
Parents and caregivers may begin to set clear behavioral expectations for youth in early adolescence, including sharing information and concerns about substance use. Monitoring the youth’s activities, mental health status, and any changes in mood or behavior can alert parents to issues that require increased support or intervention. Encouraging open discourse should be prioritized as an effort to reduce stigma of youth issues and increase skills in managing unhealthy behavior
Is social drinking really that big of an issue for adolescents and young adults?
Alcohol use disrupts brain development and can be harmful to growth in adolescence and young adulthood. Using alcohol increases impulsivity that can lead to risky sexual behaviors or unsafe driving. Adolescents who drink alcohol also have increased risk for addiction and substance abuse as adults.
How dangerous is vaping?
Use of vaping devices or e-cigarettes is often advertised as a safe alternative to combustible tobacco products. This is false. In addition to a concentrated dose of nicotine, a highly addictive substance, vaping juice often contains toxic chemicals and contaminants that can also lead to lung disease and long-term health issues. Adolescent use of vaping devices promotes development of addictive behaviors that can increase susceptibility to misuse of other substances.
References
-
American Academy of Pediatrics Committee on Substance Use and Prevention, Levy, S., Williams, J., Ryan, S., Gonzalez, P., Patrick, S., Quigley, J., Siqueira, L., Smith, V., & Walker, L. (2016). Substance use screening, brief intervention, and referral to treatment. Pediatrics, 138 (1). https://doi.org/10.1542/peds.2016-1210
-
American Academy of Pediatrics. Confidentiality in adolescent health care. AAP News. April 1989; 5:9
-
American Society of Addiction Medicine. (n.d.). Clinical guidelines. https://www.asam.org/quality- care/clinical-guidelines
-
Barnes, A. J., & Gold, M. A. (2012). Promoting healthy behaviors in pediatrics: Motivational interviewing. Pediatrics in Review, 33(9), e57-e68. http://doi.org/10.1542/pir.33-9-e57
-
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
-
Bechtold, J., Hipwell, A., Lewis, D., Loeber, R., & Pardini, D. (2016). Concurrent and sustained cumulative effects of adolescent marijuana use on subclinical psychotic symptoms. The American Academy of Psychiatry, 173(8), 781-789. https://doi.org/10.1176/appi.ajp.2016.15070878
-
Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB, Division of Adolescent and School Health. (2020). Youth risk behavior survey data summary & trends report 2009–2019. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/YRBSDataSummaryTrendsReport2019- 508.pdf
-
Centers for Disease Control and Prevention. (2020). Youth risk behavior survey data. www.cdc.gov/yrbs
-
Hadland, S.E., Yule, A.M., Levy, S.J., Hallett, E., Silverstein, M., & Bagley, S.M. (2021). Evidence-based treatment of young adults with substance use disorders. Pediatrics, 147(Suppl 2), S204-S214. https://doi.org/10.1542/peds.2020-023523D
-
Johnston, L. D., Miech, R. A., O’Malley, P. M., Bachman, J. G., Schulenberg, J. E., & Patrick, M. E. (2022). Monitoring the future national survey results on drug use 1975-2021: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, University of Michigan. https://dx.doi.org/10.7302/4142
-
Levy, S., & Botticelli, M. (2021). Moving to a medical model of substance use treatment of youth. Pediatrics, 147(Supplement 2), S262-S264
-
Levy, S.J., Williams, J.F., & COMMITTEE ON SUBSTANCE USE AND PREVENTION. (2016). Substance Use screening, brief intervention, and referral to treatment. Pediatrics, 138(1). https://doi.org/10.1542/peds.2016-1211
-
Maslyanskaya, S., & Alderman, E. M. (2019). Confidentiality and consent in the care of the adolescent patient. Pediatrics in Review, 40(10), 508-516. https://doi.org/10.1542/pir.2018-0040
-
Mee-Lee D., Shulman, G. D., Fishman, M. J., Gastfriend, D. R., & Miller, M. M. (Eds.). (2013). The ASAM criteria: Treatment criteria for addictive, substance-related, and co-occurring conditions (3rd ed.). Carson City, NV: The Change Companies.
-
Nackers, K., Kokotailo, P., & Levy, S. (2015). Substance abuse, general principles. Pediatrics in Review, 36(12). https://doi.org/10.1542/pir.36-12-535
-
National Academies of Sciences, Engineering, and Medicine. (2019). The promise of adolescence: realizing opportunity for all youth. Washington, DC: The National Academies Press. https://doi.org/10.17226/25388
-
Robinson, C. A., & Wilson, J. D. (2020). Management of opioid misuse and opioid use disorders among youth. Pediatrics, 145(Supplement_2), S153-S164. https://doi.org/10.1542/peds.2019-2056C
-
Ryan, S. A., Gonzalez, P. K., Patrick, S. W., Quigley, J., Siqueira, L., & Walker, L. R. (2016). Medication- assisted treatment of adolescents with opioid use disorders. Pediatrics, 138(3). https://doi.org/10.1542/peds.2016-1893
-
Sharma, B, Bruner, A., Barnett, G., & Fishman, M. (2016). Opioid use disorders. Child and Adolescent Psychiatric Clinics of North America, 25(3), 473-487. https://doi.org/10.1016/j.chc.2016.03.002
-
Substance Abuse and Mental Health Services Administration. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 national survey on drug use and health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/
-
Substance Abuse and Mental Health Services Administration. (2021). Screening and treatment of substance use disorders among adolescents. (Publication No. PEP20-06-04-008). https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP20-06-04-008.pdf
-
Volkow, N.D., Swanson, J.M., Evins, A.D., DeLisi, L.E., Meier, M., Gonzalez, R., Bloomfield, M.A., Curran, H.V., & Baler, R. (2016). Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: A review. JAMA Psychiatry. https://doi.org/10.1001/jamapsychiatry.2015.3278
-
World Health Organization (2019). International Statistical Classification of Diseases and Related Health Problems (11th ed.). https://icd.who.int/
